Central Facial Soft-Tissue Defect Following Surgical Resection: An Algorithm for Reconstruction
DOI:
https://doi.org/10.14228/jprjournal.v9i2.347Keywords:
Central Facial Defect, Soft Tissue, ReconstructiveAbstract
Background: Central facial soft tissue defect poses a unique challenge for the reconstructive surgeon. The three-dimensional properties of the aesthetic facial subunit and its related function are the goals for reconstruction. Considering the prominent social role of the face, the procedure to achieve a good quality of life for patients may cost more than a single surgery. This single-center study presents an algorithm of treatment for central facial soft tissue defect and it’s proposed classification according to the authors’ experiences.
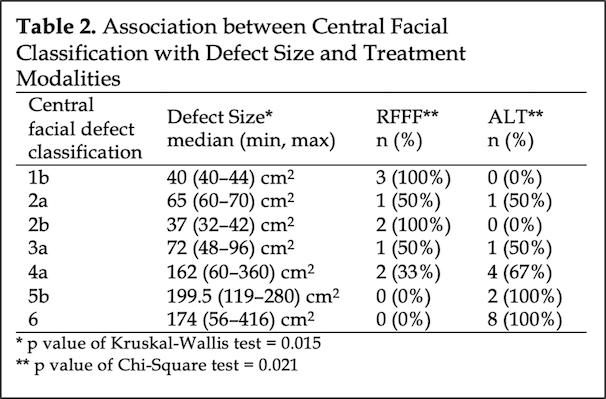
Methods: A retrospective review of medical records and photos of patients who underwent central facial soft tissue defect reconstruction in Cipto Mangunkusumo National Hospital, Jakarta, Indonesia, from 2009 to 2019. Patients who underwent free flap reconstruction were followed up, and the primary outcomes were assessed using the FACE-Q head and neck cancer (FACE-Q H&N) scale. A classification system for central facial soft tissue defect with seven subtypes (1–7) based on the facial subunit and its treatment was proposed.
Results: Twenty-five patients were included. The malignant tumor was the main etiology (88%), with basal cell carcinoma being the primary cancer pathology (64%). The average defect size was 120 cm2 (32-416 cm2) and most defects fell into subtype 6 of the classification (32%). Anterolateral thigh free flap (ALT) was the main flap of choice (64%), followed by radial forearm free flap (36%), with 92% of flaps succeeding rate from this series. All of the patients underwent at least one ancillary procedure following the reconstruction, while the average was 2 (1-6) procedures. FACE-Q H&N outcomes, especially on the appearance and appearance distress scale, showed a low to moderate score with a 72% response rate.
Conclusions: Central facial soft-tissue defect continues to challenge reconstructive surgeons. While the advances in free tissue transfer might improve the general outcomes, the numerous and costly secondary procedures do not usually end up in the best appearance. This study displayed the need for modern reconstruction modalities that provide high satisfaction in aesthetic and functional outcomes with fewer secondary procedures. Vascularized Composite Allotransplantation (VCAT) might be the future choice.
References
Pribaz JJ, Weiss DD, Mulliken JB, Eriksson E. Prelaminated free flap reconstruction of complex central facial defects. Plast Reconstr Surg. 1999;104(2):357-65; discussion 66-7. DOI: https://doi.org/10.1097/00006534-199908000-00005
Levender MM, Ratner D. Reconstructing complex central facial defects involving multiple cosmetic subunits. Facial Plast Surg. 2013;29(5):394-401. DOI: https://doi.org/10.1055/s-0033-1353380
Zhou W, He M, Liao Y, Yao Z. Reconstructing a complex central facial defect with a multiple-folding radial forearm flap. J Oral Maxillofac Surg. 2014;72(4):836 e1-4. DOI: https://doi.org/10.1016/j.joms.2013.12.027
Lago-Beack B, Acero-Sanz J. Reconstruction of midfacial defects. Front Oral Maxillofac Med 2021;3(27). DOI: https://doi.org/10.21037/fomm-2021-10
Archontaki M, Stavrianos SD, Rapidis AD. Free microvascular tissue transfer for the reconstruction of midfacial defects in oncological patients. Med Oral Patol Oral Cir Bucal. 2010;15(5):e746-51. DOI: https://doi.org/10.4317/medoral.15.e746
Cordeiro PG, Santamaria E. A classification system and algorithm for reconstruction of maxillectomy and midfacial defects. Plast Reconstr Surg. 2000;105(7):2331-46; discussion 47-8. DOI: https://doi.org/10.1097/00006534-200006000-00004
Rodriguez ED, Martin M, Bluebond-Langner R, Khalifeh M, Singh N, Manson PN. Microsurgical reconstruction of posttraumatic high-energy maxillary defects: establishing the effectiveness of early reconstruction. Plast Reconstr Surg. 2007;120(7 Suppl 2):103S-17S. DOI: https://doi.org/10.1097/01.prs.0000260728.60178.de
Shrime MG, Gilbert RW. Reconstruction of the midface and maxilla. Facial Plast Surg Clin North Am. 2009;17(2):211-23. DOI: https://doi.org/10.1016/j.fsc.2009.01.008
Cracchiolo JR, Klassen AF, Young-Afat DA, Albornoz CR, Cano SJ, Patel SG, et al. Leveraging patient-reported outcomes data to inform oncology clinical decision making: Introducing the FACE-Q Head and Neck Cancer Module. Cancer. 2019;125(6):863-72. DOI: https://doi.org/10.1002/cncr.31900
Giessler GA, Cornelius CP, Suominen S, Borsche A, Fieger AJ, Schmidt AB, et al. Primary and secondary procedures in functional and aesthetic reconstruction of noma-associated complex central facial defects. Plast Reconstr Surg. 2007;120(1):134-43. DOI: https://doi.org/10.1097/01.prs.0000263657.49956.8d
Larson DL. A Classification System and Algorithm for Reconstruction of Maxillectomy and Midfacial Defects. Plast Reconstr Surg. 2000;105(7):2347-8. DOI: https://doi.org/10.1097/00006534-200006000-00005
Moya-Plana A, Veyrat M, Honart JF, de Fremicourt K, Alkhashnam H, Sarfati B, et al. Reconstruction of maxillectomy and midfacial defects using latissimus dorsi-scapular free flaps in a comprehensive cancer center. Oral Oncol. 2019;99:104468. DOI: https://doi.org/10.1016/j.oraloncology.2019.104468
Santamaria E, Cordeiro PG. Reconstruction of maxillectomy and midfacial defects with free tissue transfer. J Surg Oncol. 2006;94(6):522-31. DOI: https://doi.org/10.1002/jso.20490
Brown JS, Shaw RJ. Reconstruction of the maxilla and midface: introducing a new classification. Lancet Oncol. 2010;11(10):1001-8. DOI: https://doi.org/10.1016/S1470-2045(10)70113-3
Solter D, Pegan A, Vagic D, Kosec A. The Role of Folded Multi-Island Vertical Rectus Abdominis Myocutaneous Flap in Reconstruction of Complex Maxillectomy and Midfacial Defects. J Craniofac Surg. 2021;32(5):1913-7. DOI: https://doi.org/10.1097/SCS.0000000000007319
Son TT, Dung PTV, Huy LA. Reconstruction of a massive facial defect with the pre-expanded free anterolateral thigh flap: A case report. Int J Surg Case Rep. 2022;90:106693. DOI: https://doi.org/10.1016/j.ijscr.2021.106693
Downloads
Published
Issue
Section
License
Copyright (c) 2022 Mohamad Rachadian Ramadan, Parintosa Atmodiwirjo, Amila Tikyayala

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors retain the copyright of the article and grant Jurnal Plastik Rekonstruksi the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License. Articles opting for open access will be immediately available and permanently free for everyone to read, download and share from the time of publication. All open access articles are published under the terms of the Creative Commons Attribution-Non-commercial-NoDerivatives (CC BY-NC-ND) which allows readers to disseminate and reuse the article, as well as share and reuse of the scientific material. It does not permit commercial exploitation or the creation of derivative works without specific permission.













