The Role of Risk Factors and Characteristic for Infantile Hemangioma at Wava Husada Hospital, Malang: Two Years of Retrospective Study
DOI:
https://doi.org/10.14228/jprjournal.v9i2.340Keywords:
Infantile Hemangioma, Age, Gender, Maternal Medication, Family History, Birth WeightAbstract
Introduction:. Infantile hemangioma is a prevalent tumor in children
Method: This research is a case control study. The data from January 1, 2019 to December 31, 2021 were processed and presented to assess the incidence and percentage of risk factors for infantile hemangioma. Univariate, bivariate and multivariate analysis was performed using Microsoft Excel SPSS 21 spreadsheet program.
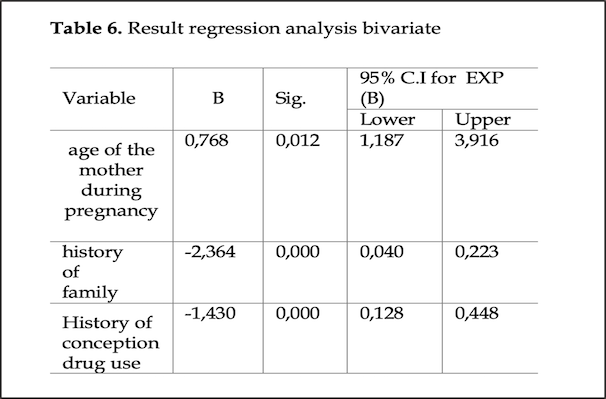
Result : Total sample in this research is 201. The risk factor for mothers aged between 22-30 years to give birth to a child with infantile hemangioma is 4.257 times greater than that of mothers aged less than 22 years. The risk factor for mothers aged more than 30 years to give birth to a child with infantile hemangioma is 9.960 times greater than that of mothers aged less than 22 years. The risk factor for patients with a family history of hemangioma was 14.175 times greater than those without a family history of infantile hemangioma or vascular abnormalities. The risk factor of using preconception drugs during pregnancy had a 4.914 times risk than those who did not use preconception drugs during pregnancy.
Conclusion: Infantile hemangioma is more common in women with average birth weight. Mothers aged 22-30 years are at greater risk of giving birth to a child with infantile hemangioma. Family history of infantile hemangioma carries a greater risk than those without. The use of medications during pregnancy is associated with a greater risk of infantile hemangioma than not.
References
Barzilay, D., Metzker, A., & Brenner, S., 2002. Some conciderations on hemangioma, SKINmed: Dermatology for the Clinician, 1(5): pp. 47 – 49. DOI: https://doi.org/10.1111/j.1540-9740.2002.01744.x
Castrén, E., Salminen, P., Vikkula, M., Pitkaranta, A., & Klockars, T., 2016. Inheritance patterns of infantile hemangioma, Pediatrics, 138(5): p. e20161623. doi: 10.1542/peds.2016- 1623. DOI: https://doi.org/10.1542/peds.2016-1623
Chang, E., Boyd, A., Nelson, C.C., Crowley, D., Law, T., Keough, K.M., Folkman, J., Ezekowitz, R.A., & Castle, V.P., 1997. Successful treatment of infant hemangiomas with interferon a-2b. Journal of Pedaitric Hematology / Oncology, 19(3): pp. 237 – 244. DOI: https://doi.org/10.1097/00043426-199705000-00011
Chen, X.D., MA, G., Chen, H., Ye, X.X., Jin, Y.B., Lin, X.X., 2013. Maternal and Perinatal Risk Factors For Infantile Hemangioma: a case-control study, Pediatri Dermatology, 30(5): pp. 457-461. doi: 10.1111/pde.12042 DOI: https://doi.org/10.1111/pde.12042
Chim, H., & Gosain, A.K., 2013. Vascular Anomalies. In: Thorne, C.H.M., Gurtner, G.C., Chung, K.C., Gosain, A., Mehrara, J.B., Rubin, J.P., & Spear, S.L., eds., Grabb and Smith’s Plastic Surgery, 7th ed., Philladelphia: Lippincott Williams & Wilkins, pp. 206 – 213.
Damanik, S.M., 2008. Klasifikasi bayi menurut berat lahir rendah dan masa gestasi. In: Kosim, M.S., Yunanto, A., Dewi, R., Sarosa, G.I., Usman, A., eds., Buku Ajar Neonatologi, 1st ed., Jakarta: Badan Penerbit IDAI, pp. 11 – 30.
Darrow, D.H., Greene, A.K., Mancini, A.J., & Nopper, A.J., 2015. Diagnosis and management of infantile hemangioma, Pediatrics, 136(4): pp. e1060 – e1104. doi: 10.1542/peds.2015-2485 DOI: https://doi.org/10.1542/peds.2015-2482
Dickison, P.R, Christou, E., & Wargon, O., 2011. A prospective study of infantile hemangiomas with a focus on incidence and risk factors, Pediatric Dermatology, 28(6): pp. 663 – 669. doi: 10.1111/j.1525- 1470.2011.01568.x. DOI: https://doi.org/10.1111/j.1525-1470.2011.01568.x
Dubois, J., Patriquin, H.B., Garel, L., Powell, J., Filiatrault, D., David, M., & Grignon, A., 1998. Soft-tissue hemangiomas in infants and children: diagnosis using Doppler sonography. American Journal of Roentgenology, 171(1): pp. 247 – 252. doi: 10.2214/ajr.171.1.9648798. DOI: https://doi.org/10.2214/ajr.171.1.9648798
Frieden, I.J., Haggstom, A.N., Drolet, B.A., Mancini, A.J., Friedlander, S.F., Boon, L., Chamlin, S.L., Baselga, E., Garzon, M.C., Nopper, A.J., Siegel, D.H., Mathes, E.W., Goddard, D.S., Bischoff, J., North, P.E., & Esterly, N.B., 2005. Infantile hemangiomas: current knowledge, future directions. Proceeding of a Research Workshop on Infantile Hemangiomas, April 7-9, 2005, Bethesda, Maryland, USA, Pediatric Dermatology, 22(5): pp. 383 – 406. doi: 10.1111/j.1525- 1470.2005.00102.x. DOI: https://doi.org/10.1111/j.1525-1470.2005.00102.x
Greco, M.F., Frieden, I.J., Drolet, B.A., Garzon, M.C., Mancini, A.J., Chamlin, S.L., Metry, D., Adams, D., Lucky, A., Wentzel, M.S., Horii, K.A., Baselga, E., McCuaig, C.C., Powell, J., Haggstrom, A., Siegel, D., Morel, K.D., Cordisco, M.R., Nopper, A.J., Krol, A., & Hemangioma Investigator Group, 2016. Infantile hemangiomas in twins: a prospective cohort study, Pediatric Dermatology, 33(2): pp. 178 – 183. doi: 10.1111/pde.12781. DOI: https://doi.org/10.1111/pde.12781
Haggstrom, A.N., & Garzon, M.C., 2012. Infantile Hemangiomas. In: Bolognia, J.L., Jorizzo, J.L., & Schaffer, J.V., eds., Dermatology, 3rd ed., Philadelphia: Elsevier, pp.1691 – 1709.
Haggstrom, A.N., Drolet, B.A., Baselga, E., Chamlin, S.L., Garzon M.C., Horii, K.A., Lucky, A.W., Mancini, A.J., Metry, D.W., Newell, B., Nopper, A.J., & Frieden, I.J., 2007. Prospective study of infantile hemangiomas: demographic, prenatal, and perinatal characteristics, The Journal of Pediatrics, 150(3): pp. 291 – 294. doi: 10.1016/j.jpeds.2006.12.003 DOI: https://doi.org/10.1016/j.jpeds.2006.12.003
Holland, K.E., & Drolet, B.A., 2010. Infantile hemangioma, Pediatric Clinics of North America, 57(5): pp. 1069 – 1083. doi: 10.1016/j.pcl.2010.07.008. DOI: https://doi.org/10.1016/j.pcl.2010.07.008
Jacobs, A.H., & Walton, R.G., 1976. The Incidence of Birthmarks in the Neonate. Pediatric, 58: pp. 218-222. DOI: https://doi.org/10.1542/peds.58.2.218
Kushner, B.J., 1999. Hemangiomas in children. The New England Journal of Medicine, 341(26): pp. 2018 – 2019. DOI: https://doi.org/10.1056/NEJM199912233412614
Li, J., Chen, X., Zhao, S., Hu, X., Chen, C., Ouyang, F., Liu, Q., Ding, R., Shi, Q., Su, J., Kuang, Y., Chang, J., Li, F., & Xie, H., 2011. Demographic and clinical characteristics and risk factors for infantile hemangioma: a Chinese case-control study, Archives of Dermatology, 147(9): pp. 1049 – 1056. doi: 10.1001/archdermatol.2011.122. DOI: https://doi.org/10.1001/archdermatol.2011.122
Mathes E.F., & Frieden I.J., 2012. Vascular Tumors. In: Goldsmith, L., Katz, S., Gilchrest, B., Paller, A., Leffell, D., & Wolff, K., eds., Fitzpatrick’s Dermatology in General Medicine, 8th ed., New York: McGraw-Hill, p. 1456 – 1469.
Mulliken, J.B., & Glowacki, J., 1982. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plastic and Reconstructive Surgery, 69(3): pp. 412 – 422. DOI: https://doi.org/10.1097/00006534-198203000-00002
Şahin, G., Düzcan-Kilimci, D., & Tanyıldız, H.G., 2017. Epidemiological features and risks of hemangiomas, The Turkish Journal of Pediatrics, 59(6): p. 664 – 669. doi: 10.24953/turkjped.2017.06.007. DOI: https://doi.org/10.24953/turkjped.2017.06.007
Tur, E., & Maibach, H.I., 2018. Gender and Dermatology, San Francisco: Springer International Pusblishing, pp. 1 – 309. doi: 10.1007/978-3-319-72156-9. DOI: https://doi.org/10.1007/978-3-319-72156-9
Waner, M., & Suen, J.Y., 1999. A classification of congenital vascular lesions. In: Waner, M., & Suen, J.Y., eds., Hemangiomas and Vascular Malformations of the Head and Neck. NewYork: Wiley-Liss, pp. 1 – 1232.
Werner, J.A., Dune, A.A., Folz, B.J., Rochels, R., Bien, S., Ramaswamy, A., & Lippert, B.M., 2001. Current concepts in the classification, diagnosis and treatment of hemangiomas and vascular malformations of the head and neck, European Archives of Oto-Rhino- Laryngology, 258(3): pp. 141 – 149. doi: 10.1007/s004050100318. DOI: https://doi.org/10.1007/s004050100318
Wu, J.K., & Ascherman, J.A., 2009. Vascular anomalies, In: Guyuron, B., Eriksson, E., Persing, J.A., Chung, K.C., Disa, J., Gosain, A., Kinney, B.M., & Rubin, J.P., eds., Plastic Surgery: Indications and Practice, 1st ed., China: Saunders Elsevier, pp. 761 – 777 DOI: https://doi.org/10.1016/B978-1-4160-4081-1.50062-X
Downloads
Published
Issue
Section
License
Copyright (c) 2022 Yuni Ariani, T Aliyatur, S W Jatmiko

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors retain the copyright of the article and grant Jurnal Plastik Rekonstruksi the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License. Articles opting for open access will be immediately available and permanently free for everyone to read, download and share from the time of publication. All open access articles are published under the terms of the Creative Commons Attribution-Non-commercial-NoDerivatives (CC BY-NC-ND) which allows readers to disseminate and reuse the article, as well as share and reuse of the scientific material. It does not permit commercial exploitation or the creation of derivative works without specific permission.













